Safer Spaces
Scotland readies to try drug consumption rooms to stem tide of epidemic

Back in 2020, Peter Krykant drove through the streets of Glasgow in a bright yellow ambulance emblazoned with red letters: “Glasgow Overdose Prevention Service.”
Inside the vehicle, a sterilized room was stocked with first-aid equipment, needles and naloxone. Its doors were open for people to inject drugs in a safer space than on the street.
After a year of running the site with a few volunteers, Krykant said the police never intervened to shut the service down.
“I just couldn’t physically continue with it anymore,” Krykant said, “but I believed that I proved the concept that it could be done.”
Peter Krykant's unsanctioned drug consumption van parked in Glasgow in 2021. Courtesy of Peter Krykant via X (formerly Twitter)
Peter Krykant's unsanctioned drug consumption van parked in Glasgow in 2021. Courtesy of Peter Krykant via X (formerly Twitter)
Now, Scottish authorities have approved a 2.3-million pound ($2.8 million) facility in Glasgow, set to open this year, that will be the first official drug consumption room in the U.K. The aim is to provide a supervised, safe and hygienic space for individuals to use illegal drugs they bring to the facility.
The Hunter Street Health and Social Care Centre, the proposed location for the drug consumption room, will join the 79 other drug consumption rooms in Europe as early as this summer. In the United States, OnPoint NYC opened the first two drug consumption rooms three years ago. Pennsylvania has none.
The Glasgow site is at the same facility where long-addicted people can access a prescription service to be given heroin under supervision.
While some believe placing a drug consumption room near the city center will further stigmatize the community, NHS Greater Glasgow and Clyde’s medical director Dr. Saket Priyadarshi said placing the service in areas where people openly use drugs is a way to ensure the facility will get used. A report from the Glasgow City Health and Social Care Partnership estimated 400 to 500 people inject drugs in public places around the downtown area on a regular basis.
“The community here feel quite stigmatized,” Priyadarshi said. “They’re a quite traumatized community because this is a community around here that was really affected by poverty and deprivation, high rates of unemployment.
“They get the worst headlines.”
Priyadarshi said 24 people now use the heroin-assisted treatment services at the Hunter Street Health and Social Care Centre — a number he hopes will rise to 40.
After a patient enters the center, a pharmacy team member prepares the prescribed diamorphine for the patient. The patient is able to sit in one of the four booths, each of which face a mirror, and inject themselves under the supervision of medical professionals.

Four seats are separated into booths for people who use drugs to inject under medical supervision. Photo by Olivia Estright
Four seats are separated into booths for people who use drugs to inject under medical supervision. Photo by Olivia Estright
Patients are then able to stay, gather themselves, have a cup of tea or coffee and engage with other services, like housing and welfare. When they’re ready to leave, they can’t take anything out with them.
Alternatively, the drug consumption room will allow individuals to bring in their own drugs for injecting, Priyadarshi said.
“People, who are currently injecting in very unhygienic environments outdoors, in public places where they’re finding a corner of the city center that’s less busy than others, behind bins, in little alleyways and little lanes, inject in a rushed matter to avoid being seen, to avoid police,” Priyadarshi said.
Priyadarshi said the facility has negotiated with the Lord Advocate, the head legal officer of Scotland, who said she’s willing to state that there’s no public interest in prosecuting people who bring drugs in to use on site.
Providing a space for people to inject themselves not only acts as a harm reduction intervention with clean equipment, it gives the individual dignity, he said.
Inside the heroin-assisted treatment service:

After receiving a referral, individuals enter the facility. Photo by Anjelica Rubin
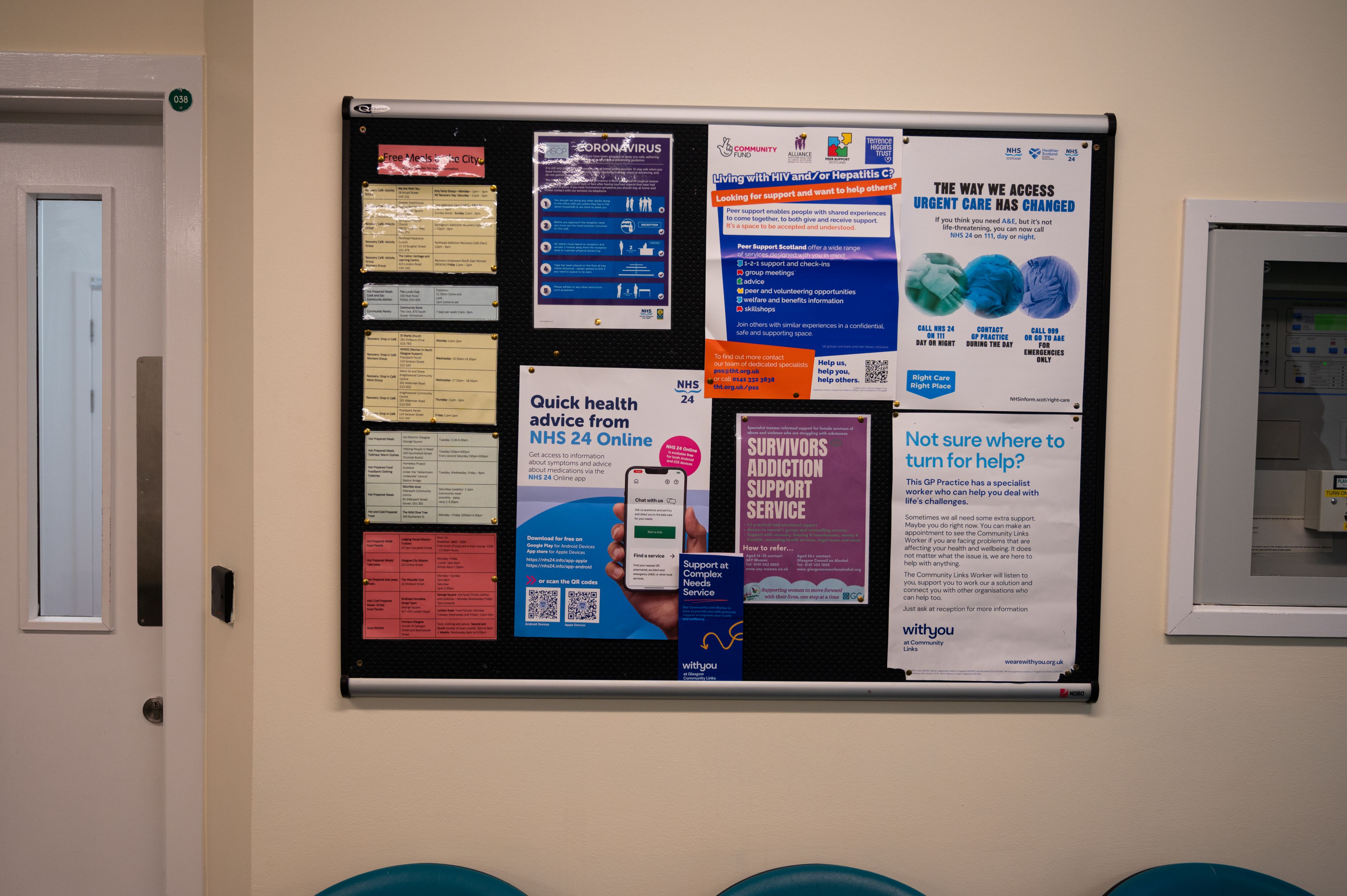
Inside the reception area, flyers provide patients with information and resources. Photo by Olivia Estright

After injecting the diamorphine, individuals place needles in the booth's bin. Photo by Olivia Estright

The diamorphine is distributed by pharmacists. Photo by Olivia Estright

Medical professionals supervise while patients inject. Photo by Anjelica Rubin
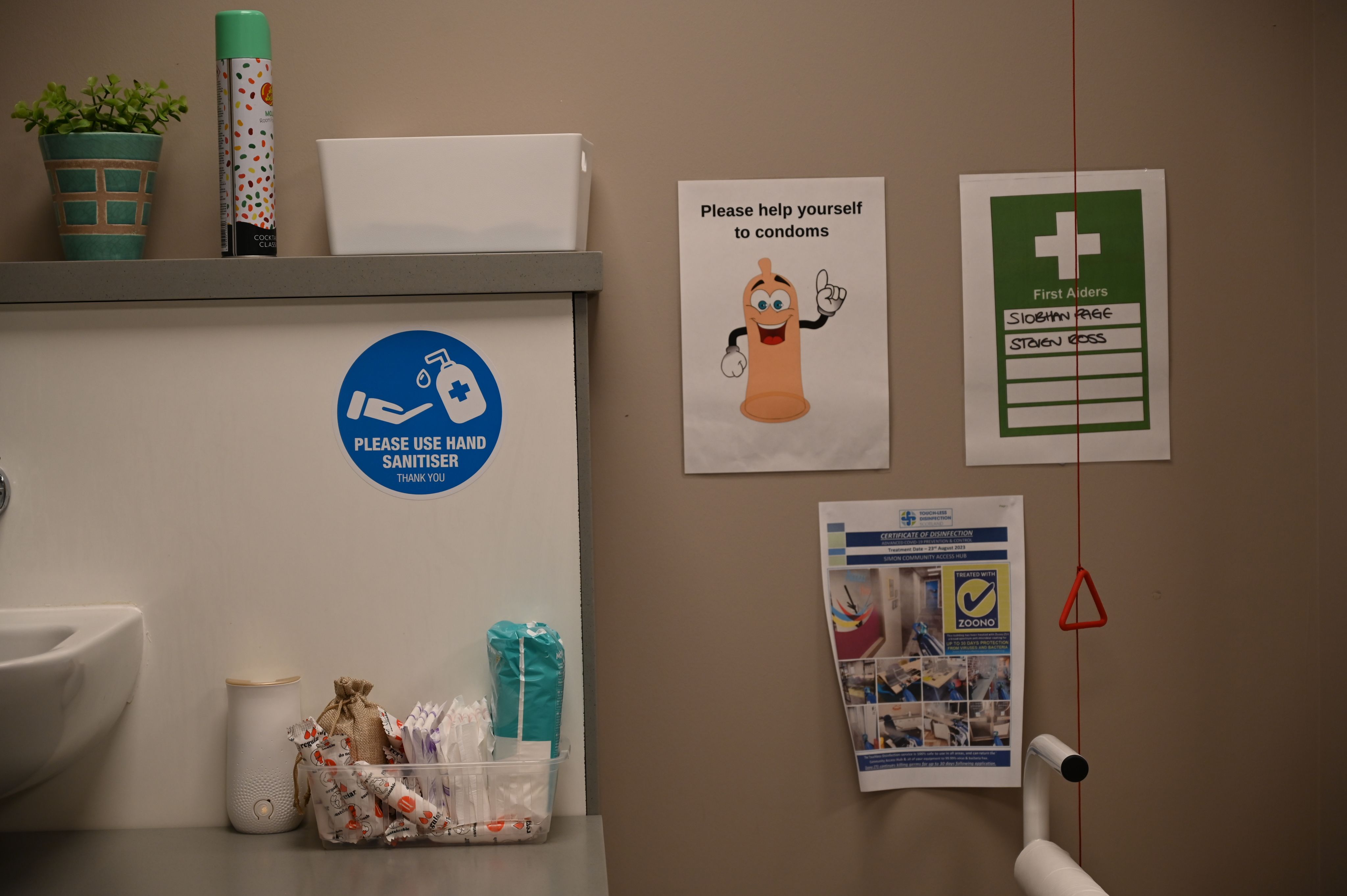
Personal supplies are offered inside the room. Photo by Anjelica Rubin
Do drug consumption rooms work?
According to the U.S. National Institutes of Health, research shows that drug consumption rooms have fostered positive impacts.
The first drug consumption room opened in 1998 in the Netherlands.
Two years later, the country introduced heroin-assisted treatment to decrease stigmatization against people who use drugs and crimes they committed. By 2008, the “epidemic” of heroin use was declared to be over by the Dutch government.
A 2019 report said the outcomes of drug consumption rooms in the Netherlands included: a decrease in public disturbance related to drug use, lowered HIV and HCV infection rates and more acceptance of the rooms by social and health care providers.
Other countries, like France, Australia and Canada, saw similarly positive results:
- In Australia, a 2010 study on the Sydney Medically Supervised Injecting Centre (MSIC) recorded an eight-year period of ambulance calls related to opioid use. The study concluded that there was a 68% decrease in monthly ambulance callouts in the MSIC vicinity.
- A study published in the Canadian Medical Association Journal considered the facility’s impact on decreased needle sharing and increased use of safe injection practices. Ultimately, the study revealed that Vancouver’s supervised injection site was associated with improved health and cost savings.
- In 2022, researchers for the International Journal of Epidemiology working in France found that drug consumption rooms had a positive impact on patients, noting they were less likely to overdose and to visit emergency rooms.
After years of discussion surrounding this harm reduction method and evidence showing no deaths inside of the consumption rooms, many point to political disagreements causing the delay. Since the U.K. government is in charge of drugs law, the Scottish government found some leeway in setting its own prosecution laws.
Ultimately, the facilities aim to assist people who are vulnerable, Priyadarshi said. He looks forward to helping more Glaswegians.
“There’s a background to everybody’s story here,” Priyadarshi said. “We think of our patients, not in a tragic way, but in a survivor’s way. … They have their own resilience, and they have their own sort of superpowers.”
Meet NHS Greater Glasgow and Clyde’s medical director Dr. Saket Priyadarshi
Listen to Priyadarshi talk about the constantly evolving drug market in Glasgow. As the service adapts to the potent drugs entering the drug market, many aspects are out of its control.
Video by Olivia Estright
